Hemoglobinuria: Unexpected Signals You Must Not Ignore
Hemoglobinuria is a rare but serious condition that may silently signal underlying health issues. While often unnoticed in early stages, certain unexpected symptoms could point to a more significant problem. Understanding these signs is essential for timely diagnosis and treatment. This article uncovers the key warning signals of hemoglobinuria and what they could mean for your health.
Hemoglobinuria represents a complex medical condition where hemoglobin appears in the urine, creating a distinctive dark red or cola-colored appearance. This phenomenon occurs when red blood cells undergo excessive destruction, overwhelming the body’s natural filtering mechanisms. The condition can manifest in various forms, with nocturnal hemoglobinuria being one of the most concerning variants that requires specialized medical intervention.
What Are Early Signs of Hemoglobinuria You Might Overlook?
Many individuals dismiss the initial symptoms of hemoglobinuria as minor inconveniences, potentially delaying crucial medical intervention. The most obvious sign is dark-colored urine, ranging from pink to deep red or brown, particularly noticeable in the morning. However, subtle symptoms often precede this dramatic change. Fatigue and weakness may develop gradually as the body struggles with decreased red blood cell counts. Some patients experience back pain, particularly in the kidney region, as the organs work overtime to filter excess hemoglobin. Shortness of breath during routine activities can indicate the body’s reduced oxygen-carrying capacity. Additionally, pale skin and cold extremities may signal developing anemia, while some individuals notice increased heart rate even during rest periods.
How Hemoglobinuria Could Indicate a Deeper Health Issue
Hemoglobinuria rarely occurs in isolation and typically signals underlying pathological processes that require immediate medical attention. Paroxysmal nocturnal hemoglobinuria (PNH) represents one of the most serious causes, involving a genetic mutation that makes red blood cells vulnerable to destruction by the body’s complement system. Autoimmune hemolytic anemia can trigger widespread red blood cell destruction, while certain infections, particularly malaria, can cause massive hemolysis. Mechanical causes include artificial heart valves or intense physical exercise that literally crushes red blood cells. Certain medications, including some antibiotics and antimalarial drugs, can precipitate hemolytic episodes in susceptible individuals. Blood transfusion reactions represent another critical cause, highlighting the importance of proper blood typing and crossmatching.
Important Diagnostic Steps for Detecting Hemoglobinuria Early
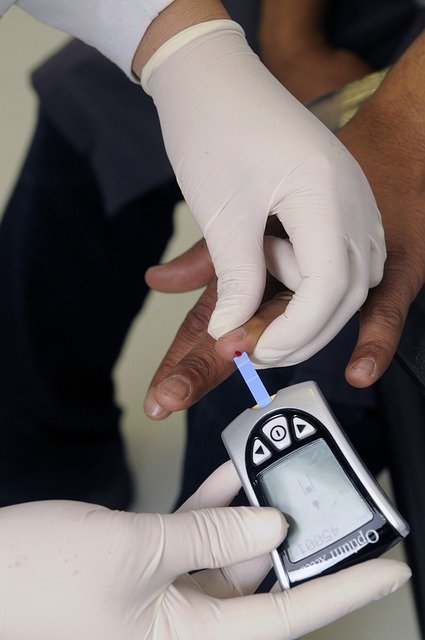
Accurate diagnosis of hemoglobinuria requires a systematic approach combining clinical evaluation with specialized laboratory testing. Initial assessment begins with a comprehensive medical history, focusing on recent medications, infections, family history of blood disorders, and symptom timeline. Physical examination reveals crucial signs including pallor, jaundice, splenomegaly, and lymph node enlargement. Laboratory evaluation starts with complete blood count to assess hemoglobin levels, red blood cell morphology, and reticulocyte count. Urinalysis confirms hemoglobin presence while ruling out other causes of red urine, such as myoglobin or blood cells. The direct antiglobulin test (Coombs test) identifies autoimmune causes, while flow cytometry can detect PNH-specific cell populations. Additional tests may include lactate dehydrogenase levels, haptoglobin measurements, and specialized genetic testing when hereditary conditions are suspected.
Myths About Hemoglobin in Urine and How to Approach Them
Several misconceptions surrounding hemoglobinuria can lead to delayed treatment and worsened outcomes. One common myth suggests that dark urine always indicates dehydration, leading patients to simply increase fluid intake without seeking medical evaluation. Another dangerous misconception claims that hemoglobinuria only affects elderly individuals, when in fact, conditions like PNH often manifest in young adults. Some believe that mild symptoms don’t require immediate attention, failing to recognize that hemoglobinuria can rapidly progress to life-threatening complications. The myth that hemoglobinuria is always painful overlooks the fact that many cases present with minimal discomfort initially. Additionally, some patients assume that clear urine between episodes means the condition has resolved, not understanding that intermittent hemoglobinuria often indicates ongoing underlying pathology requiring continuous monitoring and treatment.
Treatment Options for Nocturnal Hemoglobinuria
Treatment approaches for hemoglobinuria vary significantly depending on the underlying cause and severity of the condition. For paroxysmal nocturnal hemoglobinuria, complement inhibitors like eculizumab and ravulizumab represent breakthrough therapies that can dramatically reduce hemolysis and improve quality of life. These medications work by blocking the complement cascade that destroys defective red blood cells. Supportive care includes folic acid supplementation to support red blood cell production and iron replacement therapy when deficiency develops. Severe cases may require blood transfusions to maintain adequate hemoglobin levels, though this approach carries risks of iron overload and alloimmunization. For autoimmune causes, corticosteroids and immunosuppressive agents can reduce red blood cell destruction. Bone marrow transplantation remains the only curative option for PNH, though it’s typically reserved for severe cases due to associated risks. Preventive measures include avoiding known triggers, maintaining up-to-date vaccinations to prevent infections that could precipitate hemolytic crises, and regular monitoring with hematology specialists.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Recognizing and addressing hemoglobinuria requires vigilance from both patients and healthcare providers. Early detection through awareness of subtle symptoms, combined with prompt diagnostic evaluation and appropriate treatment, can prevent serious complications and improve long-term outcomes. The complexity of this condition underscores the importance of specialized hematological care and ongoing research into more effective therapeutic approaches.




