Hemoglobinuria:- Unexpected Signals You Must Not Ignore
Hemoglobinuria is a rare but serious condition that may silently signal underlying health issues. While often unnoticed in early stages, certain unexpected symptoms could point to a more significant problem. Understanding these signs is essential for timely diagnosis and treatment. This article uncovers the key warning signals of hemoglobinuria and what they could mean for your health.
Hemoglobinuria represents a medical condition where hemoglobin appears in urine due to excessive breakdown of red blood cells. Unlike hematuria, where intact red blood cells are present in urine, hemoglobinuria involves the release of hemoglobin protein itself. This distinction is crucial for accurate diagnosis and treatment. The condition can arise from various causes, including autoimmune disorders, infections, certain medications, and inherited blood disorders. Understanding the warning signs and seeking timely medical evaluation can prevent serious complications and guide appropriate treatment strategies.
What Are Early Signs of Hemoglobinuria You Might Overlook?
The earliest indicators of hemoglobinuria often appear subtle and easily dismissed. Dark brown, cola-colored, or reddish urine represents the most visible sign, typically noticed first thing in the morning when urine is most concentrated. Many individuals mistakenly attribute this discoloration to inadequate hydration or consumption of certain foods like beets or berries. However, hemoglobinuria-related discoloration persists despite increased fluid intake and dietary modifications.
Beyond urine color changes, individuals may experience fatigue and weakness due to anemia resulting from red blood cell destruction. Some people report abdominal or back pain, particularly in cases related to paroxysmal nocturnal hemoglobinuria. Jaundice, characterized by yellowing of the skin and eyes, can develop as the liver processes excess hemoglobin breakdown products. Shortness of breath during routine activities may occur as oxygen-carrying capacity diminishes. These symptoms often develop gradually, making them easy to overlook or attribute to stress, aging, or other common conditions.
How Hemoglobinuria Could Indicate a Deeper Health Issue
Hemoglobinuria rarely exists as an isolated condition; it typically signals underlying health problems requiring investigation. Paroxysmal nocturnal hemoglobinuria, an acquired genetic disorder, causes complement system dysfunction leading to red blood cell destruction. This rare condition increases risks for blood clots, kidney damage, and bone marrow failure if left untreated.
Autoimmune hemolytic anemia represents another significant cause, where the immune system mistakenly attacks healthy red blood cells. Infections, particularly malaria in endemic regions, can trigger massive red blood cell breakdown. Certain medications, including some antibiotics and antimalarial drugs, may induce hemolysis in susceptible individuals, particularly those with glucose-6-phosphate dehydrogenase deficiency.
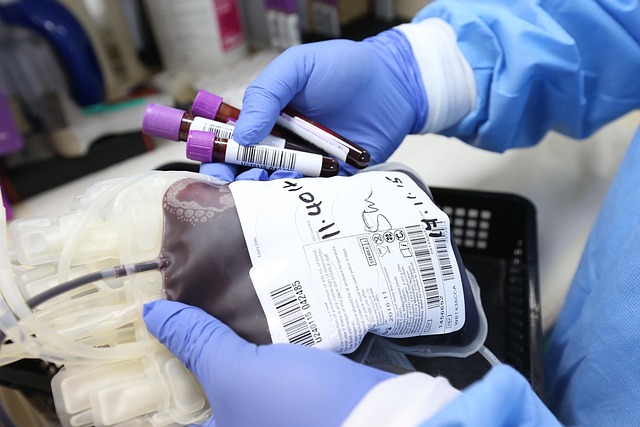
March hemoglobinuria affects athletes and military personnel following repetitive foot strikes during running or marching, causing mechanical red blood cell damage. Transfusion reactions, though rare with modern blood banking practices, can produce severe hemolysis. Exposure to toxins, snake venom, or severe burns may also precipitate hemoglobinuria. Each underlying cause requires specific diagnostic approaches and tailored treatment protocols.
Important Diagnostic Steps for Detecting Hemoglobinuria Early
Accurate diagnosis begins with comprehensive urinalysis, which detects hemoglobin presence through chemical testing and microscopic examination. The absence of intact red blood cells under microscopy despite positive hemoglobin testing confirms hemoglobinuria rather than hematuria. Laboratory evaluation includes complete blood count to assess anemia severity, reticulocyte count to measure bone marrow response, and peripheral blood smear examination to identify abnormal red blood cell shapes.
Serum testing measures lactate dehydrogenase levels, which elevate during hemolysis, alongside haptoglobin levels that decrease as this protein binds free hemoglobin. Bilirubin measurements help assess hemoglobin breakdown product accumulation. Direct antiglobulin test (Coombs test) identifies antibodies attached to red blood cells in autoimmune cases. Flow cytometry can diagnose paroxysmal nocturnal hemoglobinuria by detecting deficient surface proteins on blood cells.
Kidney function tests evaluate potential damage from hemoglobin filtering through renal tubules. Genetic testing may be warranted for inherited conditions like glucose-6-phosphate dehydrogenase deficiency or sickle cell disease. Bone marrow biopsy becomes necessary when underlying hematologic disorders are suspected. Early diagnostic intervention prevents progression to kidney failure, thrombosis, or severe anemia requiring emergency intervention.
Myths About Hemoglobin in Urine and How to Approach Them
Several misconceptions surround hemoglobinuria, potentially delaying appropriate medical care. A common myth suggests that occasional dark urine always results from dehydration and requires only increased water intake. While dehydration concentrates urine, persistent discoloration despite adequate hydration demands medical evaluation. Another misconception holds that hemoglobinuria only affects older adults, yet conditions like glucose-6-phosphate dehydrogenase deficiency and paroxysmal nocturnal hemoglobinuria can affect younger individuals.
Some believe that hemoglobinuria and hematuria are interchangeable terms, leading to confusion about underlying causes and appropriate treatments. Understanding that hemoglobinuria involves hemoglobin protein rather than intact red blood cells clarifies why different diagnostic approaches are necessary. The myth that hemoglobinuria always presents with obvious symptoms overlooks cases where laboratory abnormalities precede noticeable signs.
Another widespread belief suggests that dietary changes alone can resolve hemoglobinuria. While nutrition supports overall health, addressing underlying causes requires medical intervention, potentially including immunosuppressive therapy, complement inhibitors, or blood transfusions depending on the specific diagnosis. Some individuals mistakenly assume that hemoglobinuria always indicates kidney disease, when in fact the kidneys are often secondary victims of red blood cell destruction occurring elsewhere in the body.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Recognizing hemoglobinuria symptoms and understanding their potential significance enables individuals to seek timely medical evaluation. While some causes are benign and self-limiting, others require ongoing management to prevent serious complications. Modern diagnostic techniques allow precise identification of underlying conditions, guiding targeted treatment approaches. Awareness of early warning signs, combined with prompt medical consultation when symptoms appear, optimizes outcomes and prevents progression of potentially serious hematologic and systemic disorders. Regular follow-up with healthcare providers ensures appropriate monitoring and adjustment of treatment strategies as needed.




